Abstract
Background:
Myelodysplastic syndrome (MDS) is a pre-malignant condition characterized by ineffective hematopoiesis, cytopenias and potential to transform into acute leukemia. Acute myeloid leukemia (AML) is a hematological malignancy deriving from myeloid progenitor cells. About one quarter of patients fail to respond to initial therapy (refractory AML). In addition, around 50% of initial responders relapse after a transient remission (relapsed AML). Commonly used salvage chemotherapy regimens include FLAG, FLAG-Ida, HIDAC and Hypomethylating agents (HMA) with or without Venetoclax.
In patients who are ineligible for transplant or with poor functional status and in relapsed/refractory cases, treatment options are minimal. However recent data from Western countries has shown promising results with HMA plus Venetoclax in such patients. No such data is available from Pakistan.
Objectives:
To assess response of HMA plus Venetoclax in patients with AML and MDS treated at Armed Forces Bone Marrow Transplant Center, Rawalpindi, Pakistan.
Methods:
Study design: Single arm observational prospective study
Research Setting: Armed Forces Bone Marrow Transplant Center, Rawalpindi, Pakistan.
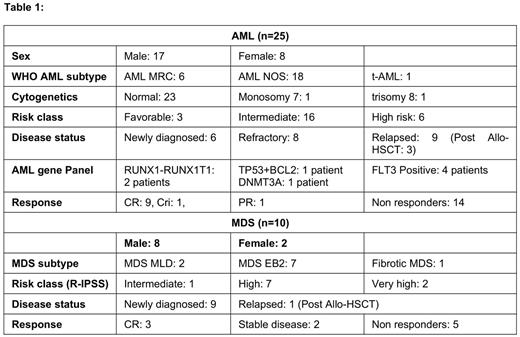
Study population: Cases included in study were patients of AML and MDS who received HMA plus Venetoclax. A total of 35 patients (25 AML, 10 MDS) were found eligible and included in the final analysis. The primary outcome measured was response to HMA plus Venetoclax.
Results:
Out of 25 AML patients 17 (68%) were male and 8 (32%) were female. Median age of patients was 44 (range 20-67). Six (24%) patients had AML MRC, 18 (72%) had AML NOS which included 2 (8%) AML-M0, 1 (4%) AML-M1, 9 (36%) AML-M2, 3 (12%) AML-M4 and 3 (12%) patients with AML-M5 while other 3 patients included 1 (4%) patient each of t-AML and AML transformed from Fanconi anemia and aplastic anemia. One (4%) AML-M2 patient had Monosomy 7 and 1 (4%) AML-M5 had trisomy 8. Three (12%), 16 (64%) and 6 (24%) patients were categorized into favorable, intermediate and high risk respectively. Nine (36%) had relapsed disease including 3 (12%) who had relapsed after allogenic HSCT, 8 (32%) had refractory disease while 7 (28%) were unfit for intensive chemotherapy due to advanced age or poor functional status. Median number of HMA+ Venetoclax cycles given were 3 (range 1-16). Overall response rate (ORR) was 44% (n=11), including 9 (36%) patients with CR and 1 (4%) with CRi. One (4%) patient had partial response (PR). Fourteen (56%) patients were non-responders. Of the 10 patients who responded, 6 (24%) achieved remission after 2 cycles while other 4 achieved remission, 1 (4%) patient each, after 1, 3, 5 and 6 cycles. Two (8%) patients underwent allogenic HSCT after achieving remission, including 1 (4%) who had relapsed after first HSCT and underwent second HSCT after achieving CR with HMA+Venetoclax.
Out of 10 MDS patients 8 (80%) were male and 2 (20%) were female. Median age of patients was 51 (range 29-71). Two (25%) patients had MDS-MLD, 6 (60%) MDS-EB2 and 2 (20%) had fibrotic MDS. One (10%), 7 (70%) and 2 (20%) patients had intermediate, high and very high risk disease (as per R-IPSS score) respectively. One (10%) patient had relapsed after allogenic HSCT. Median no of cycles of HMA+Venetoclax given were 2 (range 1-6). Three (30%) patients achieved CR (after 2 cycles each), 2 (20%) had stable disease and 5 (50%) patients were non-responders. Two (20%) patients underwent allogenic HSCT after receiving HMA+Venetoclax (Table:1)
Common side effects noted were prolonged cytopenias, febrile neutropenia and infections (cellulitis, perianal infections and fungal infections). No treatment related mortality was noted.
Conclusion:
HMA plus Venetoclax is effective treatment regimen in relapsed/ refractory AML and MDS, however our population shows inferior results as compared to Western population and further large randomized controlled trials are needed to validate this observation.
Key Words:
Relapsed AML, refractory AML, MDS, salvage chemotherapy, Hypomethylating agents, Venetoclax
Research funding: None
Word count: 691
Presentation type: Oral
Category: Acute Leukemia/ Myelodysplastic syndrome
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal